Abstract
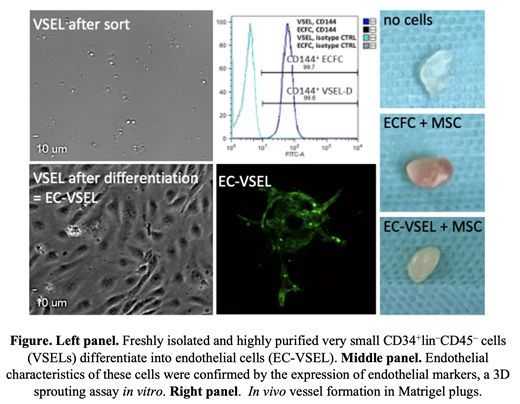
Background. Human Very small embryonic-like stem cells (VSELs) are CD133 + CD34 + small dormant stem cells with properties of self-renewal and multipotential ability to differentiate in the three-germ layers (Circulation Research 2019; 124: 208-210) and currently, more than 40 independent groups worldwide who have carefully followed the multicolor-staining cell-sorting strategy described by us (Current Protocols in Cytometry 2010 , 9.29.1-9.29.15). We have previously reported that human bone marrow (BM)-derived VSELs are able to give rise to vessel formation and endothelial differentiation (Thrombosis and Haemostasis 2015 ; 113 : 1084-1094) and several independent groups confirmed our data with human, mouse, or rat VSELs. Thus, VSELs are a promising source in regenerative medicine for the treatment of vascular diseases. Aim of the study. We aimed to develop an in vitro expansion and differentiation protocol of VSELs into endothelial cells (EC-VSELs) that will provide a clinically relevant cell therapy product without ethical problems and undesirable side effects. Materials and Methods. Highly purified by FACS from umbilical cord blood (UCB), VSELs were sorted as very small lineage-negative, CD45 -, CD34 + cells and then cultured and expanded into EC-VSELs in pro-angiogenic medium supplemented with mesodermal differentiation factors followed by stimulation by endothelial differentiation factors in the presence of UM171 and nicotinamide acid. In parallel, for comparison we expanded ECFCs from MNCs isolated from the same UCB units. The endothelial nature of the expanded VSEL-derived ECs (EC-VSELs) was tested by the expression of typical EC markers as well as by in vitro and in vivo functional angiogenic assays. Results. We report here for the first time a multistep differentiation strategy of highly purified UCB-derived VSELsThese cells after isolation by FACS were small and round, then in the presence of GSK3b inhibitor and BMP4 inducing mesodermal differentiation and high VEGF concentration to induce endothelial differentiation, VSELs enlarged and displayed extended morphology and acquired a characteristic cobblestone morphology. Finally, we have obtained a high number of cells with typical morphology of endothelial cells (EC-VSELs). By inhibiting potential mesodermal transition using TGFb inhibitor, EC-VSELs had a comparable morphology to primary human ECFCs and were characterized by tight junctions, caveolae, and Weibel-Palade Bodies, as demonstrated by transmission electron microscopy analysis of cell cultures conducted on fibrin network on the top of pericardial membranes. ECFCs differentiation was confirmed by analyzing the expression of endothelial markers by flow cytometry, and EC-VSELs were positive for PECAM1, VE-cadherin, VEGFR2, and endoglin. EC-VSELs as compared to ECFCs presented the same levels of expression of all these endothelial markers. What is important at the same time, EC-VSELs, as well as ECFCs, were negative for mesodermal marker Thy-1, confirming their endothelial phenotype. Migration properties of EC-VSELs were studied in basal conditions or in pro-angiogenic conditions using two in vitro models: wound healing assay and Trans well migration assay, and in both models EC-VSELs migration properties were similar to those of ECFCs. Next, we compared paracrine activity by evaluating growth factor and cytokine secretion profile of EC-VSELs, and noticed that the cytokine secretion by expanded VSELs was comparable to that of ECFCs. Moreover, the formation of pseudo-tubes was similar with both conditioned media. Finally, we have assessed the angiogenic capacity of EC-VSELs with a 3D in vitro sprouting assay and in vivo Matrigel plug assay. EC-VSELs display angiogenic properties but with lower potential in comparison with ECFCs which could be explained by their more primitive potential and most likely they need more time to be fully specified into the endothelial lineage. Conclusions. Based on our novel intriguing data, showing that highly purified VSELs expand efficient by employing a two-step differentiation protocol in the presence of UM171 and nicotinamide to EC-VSELs and acquire the same endothelial morphology, phenotype, and secretory potential as ECFCs as well as form functional vessels in in vitro and in vivo angiogenic assays, they could become an alternative source of ECFCs to treat vascular diseases.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal